【1.18】被抗原激活的淋巴细胞在外周淋巴器官中增殖,产生效应细胞和免疫记忆
淋巴细胞受体库的巨大多样性意味着通常会有一些淋巴细胞携带任何特定外来抗原的受体。最近的实验表明,这一数字可能是每只小鼠几百只,当然不足以对病原体产生反应。为了产生足够的抗原特异性效应淋巴细胞以抵抗感染,首先激活具有适当受体特异性的淋巴细胞以进行增殖。只有当产生了大量相同细胞克隆后,这些细胞才能最终分化为效应细胞,这一过程需要4-6天。这意味着对病原体的适应性免疫反应发生在最初感染发生并被先天免疫系统检测到近一周后
当在活化的抗原呈递细胞上识别其特定抗原时,原始淋巴细胞停止迁移,细胞核和细胞质的体积增加,新的mRNA分子和新的蛋白质合成。几个小时内,细胞看起来完全不同,被称为淋巴母细胞。分裂的淋巴母细胞能够在3-5天的过程中每24小时复制两到四次,这样单个幼稚的淋巴细胞就可以产生大约1000个具有相同特异性的子细胞的克隆。然后这些细胞分化为效应细胞。对于B细胞,分化的效应细胞是分泌抗体的浆细胞。在T细胞的情况下,效应细胞是细胞毒性T细胞,能够摧毁受感染的细胞,或辅助T细胞,激活免疫系统的其他细胞(参见第1-8节)
效应淋巴细胞不像幼稚淋巴细胞那样再循环。一些效应T细胞检测感染部位并从血液中迁移到感染部位;其他的留在淋巴组织中激活B细胞。一些分泌抗体的浆细胞保留在外周淋巴器官中,但大多数在淋巴结和脾脏中产生的浆细胞会迁移到骨髓并在那里定居,从而向血液系统分泌大量抗体。粘膜免疫系统中产生的效应细胞通常停留在粘膜组织内。免疫反应中克隆扩增产生的大多数淋巴细胞最终会死亡。然而,大量活化的抗原特异性B细胞和T细胞在抗原被清除后仍然存在。这些细胞被称为记忆细胞,是免疫记忆的基础。它们可以比幼稚的淋巴细胞更快地被激活,这确保了在第二次遇到病原体时能做出更迅速和有效的反应,从而通常提供持久的保护性免疫
通过比较个体对第一次或一次免疫的抗体反应与对使用相同抗原的第二次(或加强)免疫的反应,可以容易地观察到免疫记忆的特征。如图1.25所示,第二抗体反应发生在较短的滞后期之后,并达到明显高于第一反应的水平。在二次反应期间,抗体也可以获得更高的抗原亲和力或结合强度,这是因为一个叫做亲和成熟的过程(affinity maturation),它发生在B细胞卵泡内的特殊生发中心(见第1-16节)。重要的是,辅助T细胞是亲和力成熟过程所必需的,但T细胞受体不经历亲和力成熟。与幼稚T细胞相比,记忆T细胞显示出较低的激活阈值,但这是细胞反应性变化的结果,而不是因为受体的变化。我们在第10章中描述了抗体亲和力成熟的机制。
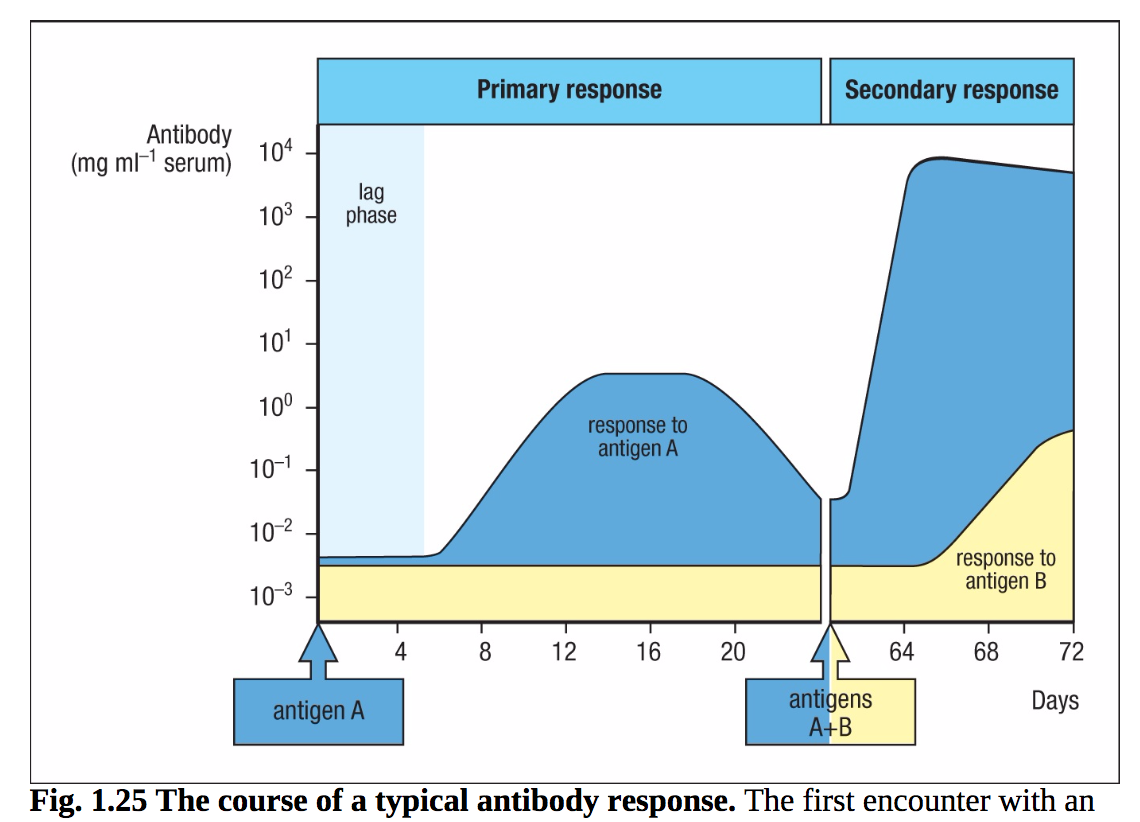
图1.25典型抗体反应的过程。初次接触抗原会产生初级反应。在时间零点引入的抗原A在血清中遇到的特异性抗体很少。在滞后期(浅蓝色)后,出现针对抗原a的抗体(深蓝色);它的浓度上升到一个平台,然后逐渐下降,这是典型的初级反应。当检测血清对另一种抗原B(黄色)的抗体时,几乎没有预设。当动物后来被抗原a和B的混合物免疫时,会对a产生非常迅速和强烈的抗体二次反应,这说明了免疫记忆。这是初次接种疫苗后注射加强针的主要原因。注意,对B的反应类似于对A的主要反应,因为这是首次遇到抗原B。
免疫记忆的细胞基础是对激发抗原具有特异性吸引力的细胞的克隆扩增和克隆分化,因此记忆完全是抗原特异性的。正是免疫记忆使疫苗接种成功,并防止被适应性免疫反应成功击退的病原体再次感染。在第11章中,我们将回到免疫记忆,这也许是适应性免疫最重要的生物学后果
总结
而先天免疫系统依赖于不变的模式识别受体来检测常见的微生物结构或它们造成的损害,适应性免疫系统释放一系列抗原受体,以识别特定于个体病原体的结构。这一特征提供了具有更高灵敏度和特异性的适应性免疫。抗原反应性淋巴细胞的克隆扩增也赋予了免疫记忆的特性,从而增强了对相同病原体再次感染的保护。
适应性免疫依赖于两种主要类型的淋巴细胞。B细胞在骨髓中成熟,是循环抗体的来源。T细胞在胸腺中成熟,并识别由感染细胞或提呈细胞上的MHC分子提供的病原体肽。适应性反应包括选择和扩增携带识别外来抗原的受体的淋巴细胞克隆。这种克隆选择为理解适应性免疫应答的所有关键特征提供了理论框架
每个淋巴细胞携带具有单一抗原特异性的细胞表面受体。这些受体是通过可变受体基因片段的随机重组和不同可变蛋白链的配对产生的:免疫球蛋白中的重链和轻链或T细胞受体的两条链。淋巴细胞的大量抗原受体几乎可以识别任何抗原。当先天免疫反应无法消除新的感染,并且活化的抗原呈递细胞(通常是携带病原体抗原和共刺激受体的树突状细胞)迁移到引流淋巴组织时,适应性免疫就会启动。
免疫反应在几个外周淋巴器官中启动。脾脏是血液传播感染的过滤器。引流各种组织的淋巴结以及粘膜相关和肠道相关的淋巴组织(MALT和GALT)被组织成特定区域,其中T和B细胞可以被抗原呈递细胞或辅助T细胞有效激活。当循环淋巴细胞在外周淋巴器官中遇到相应的抗原时,它会增殖,其克隆后代会分化为效应T淋巴细胞和B淋巴细胞,从而消除感染性病原体。这些增殖的淋巴细胞的一部分分化为记忆细胞,一旦再次遇到同样的病原体,就可以对其做出快速反应。这些识别、发展和分化过程的细节构成了本书三个中心部分的主要材料
词汇
-
immunological memory :The ability of the immune system to respond more rapidly and more effectively on a second encounter with an antigen. Immunological memory is specific for a particularantigen and is long-lived.
-
B lymphocytes (B cells) :One of the two types of antigen-specific lymphocytes responsible for adaptive immune responses, the other being the T cells. The function of B cells is to produce antibodies. B cells are divided into two classes. Conventional B cells have highly diverse antigen receptors and are generated in the bone marrow throughout life, emerging to populate the blood and lymphoid tissues. B-1 cells have much less diverse antigen receptors and form a population of self-renewing B cells in the peritoneal and pleural cavities.
-
T lymphocytes (T cells) : One of the two types of antigen-specific lymphocytes responsible for adaptive immune responses, the other being the B cells. T cells are responsible for the cell-mediated adaptive immune reactions. They originate in the bone marrow but undergo most of their development in the thymus. The highly variable antigen receptor on T cells is called the T-cell receptor and recognizes a complex of peptide antigen bound to MHC molecules on cell surfaces. There are two main lineages of T cells: those carrying αβ receptors and those carrying γδ receptors. Effector T cells perform a variety of functions in an immune response, acting always by interacting with another cell in an antigen-specific manner. Some T cells activate macrophages, some help B cells produce antibody, and some kill cells infected with viruses and other intracellular pathogens.
-
naive lymphocytes : T cells or B cells that have undergone normal development in the thymus or the bone marrow but have not yet been activated by foreign (or self) antigens. effector lymphocytes The cells that differentiate from naive lymphocytes after initial activation by antigen and can then mediate the removal of pathogens from the body without further differentiation. They are distinct from memory lymphocytes, which must undergo further differentiation to become effector lymphocytes.
-
immunoglobulin (Ig) : The protein family to which antibodies and B-cell receptors belong.
-
membrane immunoglobulin (mIg): Transmembrane immunoglobulin present on B cells; it is the B-cell receptor for antigen.
-
surface immunoglobulin (sIg): The membrane-bound immunoglobulin that acts as the antigen receptor on B cells.
-
T-cell antigen receptor, T-cell receptor (TCR) The cell-surface receptor for antigen on T lymphocytes. It consists of a disulfide-linked heterodimer of the highly variable α and β chains in a complex with the invariant CD3 and ζ proteins, which have a signaling function. T cells carrying this type of receptor are often called αβ T cells. An alternative receptor made up of variable γ and δ chains is expressed with CD3 and ζ on a subset of T cells.
-
T-cell antigen receptor, T-cell receptor (TCR) : The cell-surface receptor for antigen on T lymphocytes. It consists of a disulfide-linked heterodimer of the highly variable α and β chains in a complex with the invariant CD3 and ζ proteins, which have a signaling function. T cells carrying this type of receptor are often called αβ T cells. An alternative receptor made up of variable γ and δ chains is expressed with CD3 and ζ on a subset of T cells.
-
plasma cells: Terminally differentiated activated B lymphocytes. Plasma cells are the main antibodysecreting cells of the body. They are found in the medulla of the lymph nodes, in splenic red pulp, in bone marrow, and in mucosal tissues.
-
regulatory T cells (Treg cells): Effector CD4 T cells that inhibit T-cell responses and are involved in controlling immune reactions and preventing autoimmunity. Several different subsets have been distinguished, notably the natural regulatory T-cell lineage that is produced in the thymus, and the induced regulatory T cells that differentiate from naive CD4 T cells in the periphery in certain cytokine environments.
-
memory cells : B and T lymphocytes that mediate immunological memory. They are more sensitive to antigen than are naive lymphocytes and respond rapidly on reexposure to the antigen that originally induced them.
-
memory cells: B and T lymphocytes that mediate immunological memory. They are more sensitive to antigen than are naive lymphocytes and respond rapidly on reexposure to the antigen that originally induced them.
-
constant region (C region): That part of an immunoglobulin or a T-cell receptor that is relatively constant in amino acid sequence between different molecules. Also known as the Fc region in antibodies. The constant region of an antibody determines its particular effector function. Cf. variable region.
-
fragment crystallizable region: The carboxy-terminal halves of the two heavy chains of an IgG molecule disulfidebonded to each other by the residual hinge region. It is produced by cleavage of IgG by papain. In the complete antibody this portion is often called the Fc region.
-
variable region (V region): The region of an immunoglobulin or T-cell receptor that is formed of the aminoterminal domains of its component polypeptide chains. These are the most variable parts of the molecule and contain the antigen-binding sites. Cf. constant region.
-
antigen-binding site: The site at the tip of each arm of an antibody that makes physical contact with the antigen and binds it noncovalently. The antigen specificity of the site is determined by its shape and the amino acids present.
-
antigenic determinant: That portion of an antigenic molecule that is bound by the antigen-binding site of a given antibody or antigen receptor; it is also known as an epitope.
-
epitope: A site on an antigen recognized by an antibody or an antigen receptor. T-cell epitopes are short peptides bound to MHC molecules. B-cell epitopes are typically structural motifs on the surface of the antigen. Also called an antigenic determinant.
-
MHC molecules: Highly polymorphic cell-surface proteins encoded by MHC class I and MHC class II genes involved in presentation of peptide antigens to T cells. They are also known as histocompatibility antigens.
-
major histocompatibility complex (MHC): A cluster of genes on human chromosome 6 that encodes a set of membrane glycoproteins called the MHC molecules. The MHC also encodes proteins involved in antigen processing and other aspects of host defense. The genes for the MHC molecules are the most polymorphic in the human genome, having large numbers of alleles at the various loci.
-
gene segments: Sets of short DNA sequences at the immunoglobulin and T-cell receptor loci that encode different regions of the variable domains of antigen receptors. Gene segments of each type are joined together by somatic recombination to form a complete variabledomain exon. There are three types of gene segments: V gene segments encode the first 95 amino acids, D gene segments (in heavy-chain and TCRα chain loci only) encode about 5 amino acids, and J gene segments encode the last 10–15 amino acids of the variable domain. There are multiple copies of each type of gene segment in the germline DNA, but only one of each type is joined together to form the variable domain.
-
combinatorial diversity: The diversity among antigen receptors generated by combining separate units of genetic information, comprising two types. First, receptor gene segments are joined in many different combinations to generate diverse receptor chains; second, two different receptor chains (heavy and light in immunoglobulins; α and β, or γ and δ, in T-cell receptors) are combined to make the antigen-recognition site.
-
junctional diversity: The variability in sequence present in antigen-specific receptors that is created during the process of joining V, D, and J gene segments and which is due to imprecise joining and insertion of non-templated nucleotides at the joins between gene segments.
-
clone: A population of cells all derived from the same progenitor cell.
-
lymphocyte receptor repertoire: All the highly variable antigen receptors carried by B and T lymphocytes.
-
clonal expansion: The proliferation of antigen-specific lymphocytes in response to antigenic stimulation that precedes their differentiation into effector cells. It is an essential step in adaptive immunity, allowing rare antigen-specific cells to increase in number so that they can effectively combat the pathogen that elicited the response.
-
clonotypic: Describes a feature unique to members of a clone. For example, the distribution of antigen receptors in the lymphocyte population is said to be clonotypic, as the cells of a given clone all have identical antigen receptors.
-
clonal selection theory: The central paradigm of adaptive immunity. It states that adaptive immune responses derive from individual antigen-specific lymphocytes that are self-tolerant. These specific lymphocytes proliferate in response to antigen and differentiate into antigenspecific effector cells that eliminate the eliciting pathogen and into memory cells to sustain immunity. The theory was formulated by Frank Macfarlane Burnet and in earlier forms by Niels K. Jerne and David Talmage.
-
cellular immunology: The study of the cellular basis of immunity.
-
self antigens: The potential antigens on the tissues of an individual, against which an immune response is not usually made except in the case of autoimmunity.
-
tolerant: Describes the state of immunological tolerance, in which the individual does not respond to a particular antigen.
-
clonal deletion: The elimination of immature lymphocytes when they bind to self antigens, which produces tolerance to self as required by the clonal selection theory of adaptive immunity. Clonal deletion is the main mechanism of central tolerance and can also occur in peripheral tolerance.
-
apoptosis : A form of cell death common in the immune system, in which the cell activates an internal death program. It is characterized by nuclear DNA degradation, nuclear degeneration and condensation, and the rapid phagocytosis of cell remains. Proliferating lymphocytes experience high rates of apoptosis during their development and during immune responses.
-
programmed cell death: A form of cell death common in the immune system, in which the cell activates an internal death program. It is characterized by nuclear DNA degradation, nuclear degeneration and condensation, and the rapid phagocytosis of cell remains. Proliferating lymphocytes experience high rates of apoptosis during their development and during immune responses.
-
anergy: A state of nonresponsiveness to antigen. People are said to be anergic when they cannot mount delayed-type hypersensitivity reactions to a test antigen, whereas T cells and B cells are said to be anergic when they cannot respond to their specific antigen under optimal conditions of stimulation.
-
lymphoid tissue: Tissue composed of large numbers of lymphocytes.
-
lymphoid organs: Organized tissues characterized by very large numbers of lymphocytes interacting with a nonlymphoid stroma. The central, or primary, lymphoid organs, where lymphocytes are generated, are the thymus and bone marrow. The main peripheral, or secondary, lymphoid organs, in which adaptive immune responses are initiated, are the lymph nodes, spleen, and mucosa-associated lymphoid organs such as tonsils and Peyer’s patches.
-
thymus: A central lymphoid organ, in which T cells develop, situated in the upper part of the middle of the chest, just behind the breastbone.
-
lymph nodes: A type of peripheral lymphoid organ present in many locations throughout the body where lymphatic vessels converge.
-
spleen: An organ in the upper left side of the peritoneal cavity containing a red pulp, involved in removing senescent blood cells, and a white pulp of lymphoid cells that respond to antigens delivered to the spleen by the blood.
-
bursa of Fabricius: Lymphoid organ associated with the gut that is the site of B-cell development in chickens.
-
co-stimulatory molecules: Cell-surface proteins on antigen-presenting cells that deliver co-stimulatory signals to naive T cells. Examples are the B7 molecules on dendritic cells, which are ligands for CD28 on naive T cells.
-
antigen-presenting cells (APCs): Highly specialized cells that can process antigens and display their peptide fragments on the cell surface together with other, co-stimulatory, proteins required for activating naive T cells. The main antigen-presenting cells for naive T cells are dendritic cells, macrophages, and B cells.
-
draining lymph node: A lymph node downstream of a site of infection that receives antigens and microbes from the site via the lymphatic system. Draining lymph nodes often enlarge enormously during an immune response and can be palpated; they were originally called swollen glands.
-
afferent lymphatic vessels: Vessels of the lymphatic system that drain extracellular fluid from the tissues and carry antigen, macrophages, and dendritic cells from sites of infection to lymph nodes or other peripheral lymphoid organs.
-
follicles: An area of predominantly B cells in a peripheral lymphoid organ, such as a lymph node, which also contains follicular dendritic cells.
-
cortex: The outer part of a tissue or organ; in lymph nodes it refers to the follicles, which are mainly populated by B cells.
-
paracortical areas: The T-cell areas of lymph nodes.
-
T-cell zones: Regions of peripheral lymphoid organs that are enriched in naive T cells and are distinct from the follicles. They are the sites at which adaptive immune responses are initiated.
-
germinal centers: Sites of intense B-cell proliferation and differentiation that develop in lymphoid follicles during an adaptive immune response. Somatic hypermutation and class switching occur in germinal centers.
-
red pulp: The nonlymphoid area of the spleen in which red blood cells are broken down.
-
white pulp: The discrete areas of lymphoid tissue in the spleen.
-
periarteriolar lymphoid sheath (PALS): Part of the inner region of the white pulp of the spleen; it contains mainly T cells.
-
marginal zone: Area of lymphoid tissue lying at the border of the white pulp in the spleen.
-
marginal zone B cells: A unique population of B cells found in the spleen marginal zones; they do not circulate and are distinguished from conventional B cells by a distinct set of surface proteins.
-
mucosal immune system: The immune system that protects internal mucosal surfaces (such as the linings of the gut, respiratory tract, and urogenital tracts), which are the site of entry for virtually all pathogens and other antigens. See also mucosa-associated lymphoid tissue.
-
mucosa-associated lymphoid tissue (MALT): Generic term for all organized lymphoid tissue found at mucosal surfaces, in which an adaptive immune response can be initiated. It comprises gut-associated lymphoid tissue (GALT), nasal-associated lymphoid tissue (NALT), and bronchus-associated lymphoid tissue (BALT) (when present).
-
gut-associated lymphoid tissue (GALT): Lymphoid tissues associated with the gastrointestinal tract, comprising Peyer’s patches, the appendix, and isolated lymphoid follicles found in the intestinal wall, where adaptive immune responses are initiated.
-
tonsils: Paired masses of organized peripheral lymphoid tissue situated at the base of the tongue, in which adaptive immune responses can be initiated. They are part of the mucosal immune system. See also palatine tonsils.
-
adenoids: Paired mucosa-associated lymphoid tissue located in the nasal cavity.
-
appendix: A gut-associated lymphoid tissue located at the beginning of the colon.
-
Peyer’s patches: Organized peripheral lymphoid organs under the epithelium in the small intestine, especially the ileum, and in which an adaptive immune response can be initiated. They contain lymphoid follicles and T-cell areas. They are part of the gut-associated lymphoid tissue (GALT).
-
microfold cells: Specialized epithelial cell type in the intestinal epithelium over Peyer’s patches, through which antigens and pathogens enter from the gut.
-
M cells: Specialized epithelial cell type in the intestinal epithelium over Peyer’s patches, through which antigens and pathogens enter from the gut.
-
bronchus-associated lymphoid tissue (BALT): Organized lymphoid tissue found in the bronchi in some animals. Adult humans do not normally have such organized lymphoid tissue in the respiratory tract, but it may be present in some infants and children.
-
lamina propria: A layer of connective tissue underlying a mucosal epithelium. It contains lymphocytes and other immune-system cells.
-
lymphoblast: A lymphocyte that has enlarged after activation and has increased its rate of RNA and protein synthesis but is not yet fully differentiated.
-
primary immunization: The first encounter with a given antigen, which generates the primary adaptive immune response.
-
affinity maturation: The increase in affinity of antibodies for their specific antigen as an adaptive immune response progresses. This phenomenon is particularly prominent in secondary and subsequent immunizations.
-
B-cell antigen receptor, B-cell receptor (BCR): The cell-surface receptor on B cells for specific antigen. It is composed of a transmembrane immunoglobulin molecule (which recognizes antigen) associated with the invariant Igα and Igβ chains (which have a signaling function). On activation by antigen, B cells differentiate into plasma cells producing antibody molecules of the same antigen specificity as this receptor.
-
effector T lymphocytes, effector T cells: The T cells that perform the functions of an immune response (such as cell killing and cell activation) that clear the infectious agent from the body. There are several different subsets, each with a specific role in an immune response.
-
helper CD4 T cells, helper T cells: Effector CD4 T cells that stimulate or ‘help’ B cells to make antibody in response to antigenic challenge. TH2, TH1, and the TFH subsets of effector CD4 T cells can perform this function.
-
Fc fragment, Fc region: The carboxy-terminal halves of the two heavy chains of an IgG molecule disulfidebonded to each other by the residual hinge region. It is produced by cleavage of IgG by papain. In the complete antibody this portion is often called the Fc region.
-
heavy chain, H chain: One of the two types of protein chains in an immunoglobulin molecule, the other being called the light chain. There are several different classes, or isotypes, of heavy chain (α,δ, ε, γ, and μ), each of which confers a distinctive functional activity on the antibody molecule. Each immunoglobulin molecule contains two identical heavy chains.
-
light chain, L chain: The smaller of the two types of polypeptide chains that make up an immunoglobulin molecule. It consists of one V and one C domain and is disulfide-bonded to the heavy chain. There are two classes, or isotypes, of light chain, known as κ and λ, which are produced from separate genetic loci.
-
primary lymphoid organs: The sites of lymphocyte development; in humans, these are the bone marrow and thymus. B lymphocytes develop in bone marrow, whereas T lymphocytes develop within the thymus from bone marrow–derived progenitors. Also called the primary lymphoid organs and tissues.
-
secondary lymphoid organs: The lymph nodes, spleen, and mucosa-associated lymphoid tissues, in which adaptive immune responses are induced, as opposed to the central lymphoid organs, in which lymphocytes develop. They are also called secondary lymphoid organs and tissues.
-
lymphatic vessels, lymphatics: Thin-walled vessels that carry lymph.
-
high endothelial cells, high endothelial venules (HEVs): Specialized small venous blood vessels in lymphoid tissues. Lymphocytes migrate from the blood into lymphoid tissues by attaching to the high endothelial cells in the walls of the venules and squeezing between them.
-
secondary immunization: A second or booster injection of an antigen, given some time after the initial immunization. It stimulates a secondary immune response.
-
nasal- (or nasopharynx-) associated lymphoid tissue (NALT): Organized lymphoid tissues found in the upper respiratory tract. In humans, NALT consists of Waldeyer’s ring, which includes the adenoids and palatine and lingual tonsils, plus other similarly organized lymphoid tissue located around the pharynx. It is part of the mucosal immune system.
参考资料
- Janeway’s Immunobiology 10th edition
